In Romania, the frequency of colorectal cancer is increasing rapidly. Incidence and mortality have doubled in the last 20 years, reaching in 2000 an incidence of 17.74 /100,000 inhabitants; in 2006 there were 8240 new cases, placing Romania among the countries with an average incidence of the disease. In the last 2 years colorectal cancer has become the second leading cause of cancer deaths (after bronchopulmonary cancer, but ahead of gastric cancer), with 4,150 deaths in 2002 (19.05/100,000 places) and 4,860 deaths in 2006.
The male/female ratio is 1.3. Less than 3% of cases occur in people under 40. The incidence increases rapidly over the age of 45 and doubles with each decade of life.
Early stage bowel cancer may not show any symptoms; and some symptoms of advanced bowel cancer may also occur in people with less serious medical problems, such as haemorrhoids.
See your doctor if you notice any of the following symptoms below:
As bowel cancer progresses, it can sometimes cause bleeding inside the bowel. Eventually, this can lead to a deficiency of red blood cells in the body, a phenomenon called anaemia.
Symptoms of anaemia include fatigue and shortness of breath.
In some cases, bowel cancer can cause an obstruction in the bowel. Symptoms of intestinal obstruction include:
Cancer occurs when cells in a particular area of the body divide and multiply too quickly. This produces a piece of tissue known as a tumour.
Most cases of colon cancer first develop within the clump of cells on the inner lining of the intestine. These lumps are known as polyps. However, if you develop polyps, it doesn’t necessarily mean you’ll get bowel cancer.
It is not yet known exactly what causes cancer to develop inside the gut. However, research has shown that there are several factors that may increase the chances of developing it.
About 2/3 of people diagnosed with bowel cancer are over 60 years old.
There is evidence that bowel cancer can be passed on genetically. About 20% of people who develop bowel cancer have a close relative (mother, father, brother or sister) or a second-degree relative (grandparent, uncle or aunt) who also had colon cancer.
It is estimated that if you have a close relative with a history of bowel cancer, your risk of developing bowel cancer doubles. If you have two close relatives with a history of bowel cancer, your risk increases fourfold.
A large body of evidence suggests that a diet high in red and processed meat can increase the risk of developing colon cancer. For this reason, the Department of Health advises people who eat more than 90 grams (cooked meat weight) of red and processed meat a day to reduce their consumption to 70 grams.
There is also evidence that a diet high in fibre and low in saturated fat can help reduce the risk of bowel cancer. Oncology specialists believe this is because this type of diet encourages regular bowel movements.
People who smoke cigarettes are 25% more likely to develop bowel cancer, other cancers and heart disease than non-smokers.
A major study, called the EPIC study, showed that alcohol was associated with bowel cancer risk. Even alcohol in small amounts can put you at higher risk of developing bowel cancer. The EPIC study found that for every two units of alcohol a person drinks every day, the risk of developing bowel cancer is up to 8%.
Obesity is linked to an increased risk of bowel cancer. Obese men are 50% more likely to develop bowel cancer than people of normal weight. Highly obese men with a body mass index (BMI) of over 40 are twice as likely to develop bowel cancer.
Obese women have a slightly increased risk of developing the disease, and highly obese women are 50% more likely to develop bowel cancer than women of normal weight.
People who are sedentary have a higher risk of developing bowel cancer. You can help reduce your risk of bowel and other cancers by exercising every day. The risk can be reduced by up to a fifth if you do an hour of strenuous exercise every day or two hours of moderate exercise (such as vacuuming or walking).
Some diseases may put you at a higher risk of developing bowel cancer. People with Crohn’s disease (inflammation of the colon) are 2-3 times more likely to develop colon cancer. The risk of developing colon cancer is much higher in people with ulcerative colitis, and 1 in 20 of these people will go on to develop the disease.
There are two rare hereditary diseases that can cause bowel cancer. These are:
When you first visit your GP, he or she will ask you about your symptoms and whether you have a family history of bowel cancer.
He will then perform a physical examination which is known as a digital rectal examination (DRE).
A DRE examination is a useful way to check for a visible lump inside the rectum. It is detected in about 40-80% of rectal cancer cases.
Two tests are commonly used to confirm a diagnosis of bowel cancer:
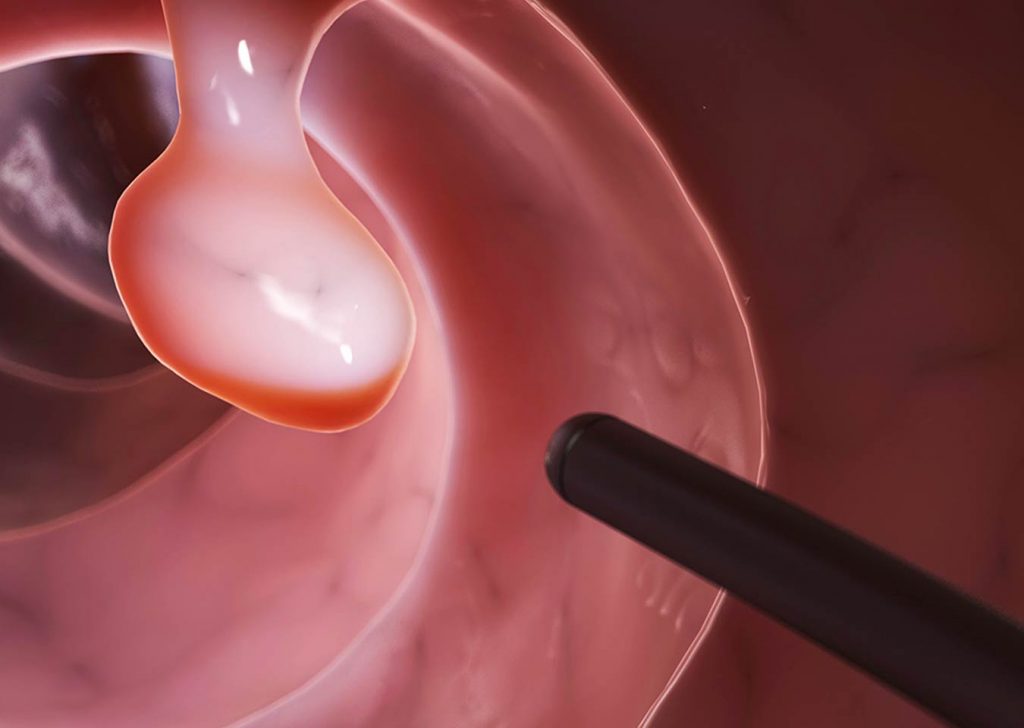
Sigmoidoscopy uses a device called a sigmoidoscope, which is a thin, flexible tube attached to a small chamber with a light.
The sigmoidoscope is inserted into the rectum and then directed up into the bowel. The camera displays images on a monitor. This allows the doctor to check for abnormal areas in the rectum or bowel that could be the result of cancer.
Sigmoidoscopy can also be used to remove small tissue samples that are suspected of being cancerous so they can be tested in the laboratory. This procedure is known as a biopsy.
Usually sigmoidoscopy is not painful, but it can be uncomfortable. Most people go home after the examination has been completed.
Colonoscopy is similar to sigmoidoscopy except that a longer tube, called a colonoscope, is used to examine the entire intestine.
The bowel must be empty when the colonoscopy is performed, so you will be given a special diet for a few days before the examination and a laxative (medication to help empty the bowel) on the morning of the examination.
You will be given a sedative to help you relax, after which the doctor will insert the colonoscope into your rectum and move it along your large intestine. As with the sigmoidoscope, the colonoscope can be used to obtain a biopsy as well as images showing any abnormal areas.
Colonoscopy takes about an hour to complete; most people can go home once they have recovered from the sedative. After the procedure, you’ll probably feel sleepy for a while, so arrange with someone to drive you home.
If the diagnosis of bowel cancer is confirmed, further tests are usually performed for two reasons:
These tests may include:
Once the above examinations and tests have been completed, it should be possible to determine the stage and grade of the cancer. Staging refers to how far the cancer has advanced. Grading refers to how aggressive and how likely the cancer is to spread.
This is a simplified guide. Stage II is divided into further categories called A and B and Stage III is divided into categories A, B and C.
There are three categories of bowel cancer:
People with colorectal cancer need to be cared for by a multidisciplinary team. This is a team of specialists working together to provide the best treatment and care and to make decisions within the Oncology Commission. Decisions will take into account:
Surgery is usually the main treatment for bowel cancer, but in about 1 in 5 cases, the cancer is too advanced to be removed by surgery and radiotherapy is used. If you have surgery, you may also need chemotherapy, radiotherapy or biological therapy, depending on your case.
If the cancer is at an early stage, it is possible to remove a small portion of the lining of the colon wall. This procedure is known as local excision.If the cancer has spread to the muscles surrounding the colon, it will usually be necessary to remove an entire portion of the colon. Partial removal of the colon is known as a colectomy.
Depending on the location of the cancer, possible surgical procedures include:
There are two ways in which colectomy can be performed:
Both techniques are considered equally effective in removing cancer and carry similar risks of complications. Laparoscopic colectomies have the advantage of a faster recovery time and involve less post-operative pain.
Laparoscopic colectomies should now be available in all hospitals performing colon cancer surgery, although not all surgeons perform this type of procedure. If you are considering colon cancer surgery using keyhole surgery, discuss this with your surgeon.
During surgery, nearby lymph nodes may also be removed. It is customary to join the ends of the bowel after colon cancer surgery, but it is extremely rare that this is not possible and a stoma is required.
In some cases, the surgeon may decide that the colon needs to be healed before it can be reconstructed, or that too much of the colon has been removed for reconstruction to be possible.
In this case, it will be necessary to find a way to remove waste material from the body without the stool passing through the anus. This is done through surgery for the stoma.
Ostomy surgery involves the surgeon cutting a small hole in the abdomen, which is known as an ostomy. There are two ways in which this procedure can be carried out.
In most cases, the stoma will be temporary and can be removed once the colon has recovered from the effects of surgery. This will take at least 9 weeks. Stoma specialist nurses are available to advise on the best place for the stoma, and on the best type of bag to cover the stoma and collect waste material.
Before a colectomy is performed, your care team will tell you whether they think the stoma procedure will be necessary and about the likelihood of needing a temporary or permanent ileostomy or colostomy.
Two general surgical procedures can be used to treat rectal cancer:
Low anterior resection is a procedure used to treat cases where the cancer is in the upper portion of the rectum. The surgeon will make an incision in the abdomen and remove the upper portion of the rectum, as well as the surrounding tissue to ensure that all lymph nodes containing cancer cells are removed. They will then place the colon in the most caudal portion of the rectum or the upper part of the anal canal. Sometimes they turn the end of the colon into an internal pouch to replace the rectum. You will probably need a temporary ostomy to allow healing time for the joint.
Abdominoperineal resection is used to treat cases where the cancer is in the most caudal portion of the rectum. In this case, it will be necessary to remove the entire rectum and surrounding muscles to reduce the risk of cancer recurrence in the same area. This involves removing the anus and also the sphincter muscles, so there is no option except to perform a permanent stoma after surgery. Bowel cancer surgeons do their best to avoid performing operations to place permanent stomas.
Most doctors prefer to administer radiotherapy before surgery because it can make it easier to remove the cancer, especially if the size and/or position of the cancer cells can make the operation difficult.
There are three ways chemotherapy can be used to treat bowel cancer:
Chemotherapy for bowel cancer usually involves taking a combination of drugs that destroy cancer cells. The drugs can be administered as a tablet (oral chemotherapy), through an infusion into the arm or chest (intravenous chemotherapy) or as a combination of the two.
Depending on the stage and grade of the cancer, a single session of intravenous chemotherapy can last from a few hours to a few days.
Most people have regular daily chemotherapy sessions for one or two weeks before taking a break from treatment for another week.
A course of chemotherapy can last up to six months depending on how well you respond to treatment.
Side effects of chemotherapy include:
These side effects should gradually pass once the treatment is over. It usually takes three to six months for hair to grow back.
Chemotherapy can also weaken the immune system, making it more vulnerable to infection. Inform your care team or doctor as soon as possible if you show possible signs of infection, including:
Medicamentele utilizate în chimioterapie pot provoca afecţiuni temporare ale spermei bărbaţilor şi ale ovulelor femeilor. Acest lucru înseamnă că pentru femeile care rămân gravide sau pentru bărbaţii care urmează să aibă un copil există un risc pentru sănătatea fetusului. Prin urmare, se recomandă utilizarea unei metode contraceptive sigure în timpul urmării unui tratament cu chimioterapie şi timp de încă un an de la finalizarea tratamentului.
There are three main ways radiotherapy can be used to treat bowel cancer. These are:
External radiotherapy is usually given daily, five days a week, with a break on weekends. Depending on the size of the tumour, you may need 1 to 5 weeks of treatment. Each radiotherapy session is short and will last only 5-10 minutes.
With the latest IMRT-VMAT technology, it is now possible to protect organs that are close to the tumour from being affected by the treatment itself.
Palliative radiotherapy is usually administered in short, daily sessions with a course ranging from 2-3 days to 10 days.
Short-term side effects of radiotherapy include:
These side effects should pass once the radiotherapy treatment is over. Inform your care team if side effects of treatment become troublesome. Often additional treatments are available to help you cope better with side effects.
Long-term side effects of radiotherapy include:
If you want to have children, it is possible to store a sample of sperm or eggs before starting treatment so that they can be used for fertility treatments in the future.
The recommended treatment plan will depend on the stage and location of the bowel cancer.