Lung cancer is the most common and most serious type of cancer. Lung cancer is the most common cancer in Romania. More than 11,000 new cases are diagnosed each year, most of them in men (8,500 cases out of 11,000).
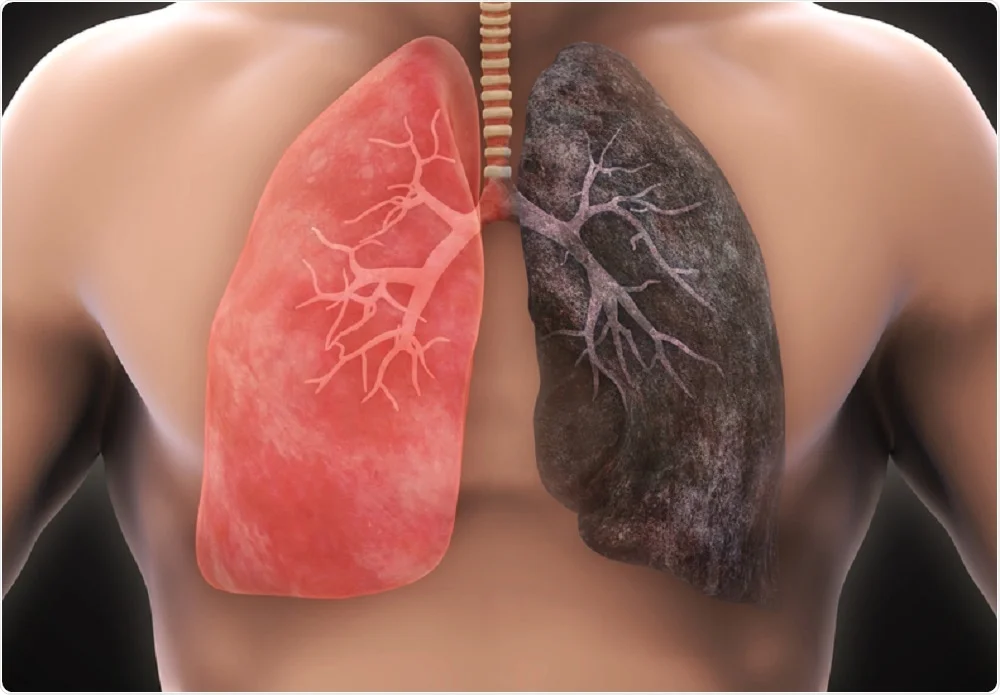
Smoking is the cause of 85-90% of lung cancers. People who smoke are 15 times more likely to die from lung cancer than people who have never smoked.
The lungs have two main purposes:
The lungs are made up of a series of sections called lobes. The left lung consists of two lobes. The right lung is larger and consists of three lobes.
Cancer that starts in the lungs is called primary lung cancer. Cancer that starts in another part of the body and spreads to the lungs is known as secondary lung cancer.
Depending on the type of cells that trigger malignant tumours, primary lung cancer is classified into 2 types:
Cigarette smoking is the biggest risk factor for lung cancer. It is responsible for 85-90% of all cases. People who smoke are 15 times more likely to die from lung cancer than people who have never smoked.
Cigarette smoke contains more than 60 different toxic substances that can lead to cancer. These substances are known carcinogens (cancer-causing).
If you smoke more than 25 cigarettes a day, you are 25 times more likely to develop lung cancer than a non-smoker.
While cigarette smoking is the biggest risk factor, the use of other tobacco products can also increase the risk of developing lung cancer and other cancers such as oesophageal and oral cancer. These products include:
Even if you don’t smoke, frequent exposure of a non-smoker to cigarette smoke (passive smoking) can increase the risk of developing lung cancer. For example, research has shown that non-smoking women living with a smoking partner are 25% more likely to develop lung cancer than a non-smoking woman cohabiting with a non-smoker.
Radon is an element that occurs through the radioactive decay of radium and is present in soil, rocks, water and atmospheric air. If it is breathed in, it can damage your lungs, especially if you are a smoker. It is estimated that radon is responsible for around 3% of all lung cancer deaths in England.
Exposure to certain chemicals and substances that are used in certain professions and industries has been linked to a slightly higher risk of developing lung cancer. These chemicals and substances include arsenic, asbestos, beryllium, cadmium, coal and coke smoke, silicon dioxide and nickel. Combining smoking with asbestos exposure increases the risk of developing the disease by 50-100 times.
If you have symptoms such as shortness of breath and a persistent, long-lasting cough, your doctor will perform some routine tests to rule out possible causes other than lung cancer, such as lung infection.
Two tests you may want to perform are:
If you coughed up blood, you should be sent straight for a chest X-ray.
Chest X-ray is usually the first investigation performed to diagnose lung cancer. Most lung tumours show up on X-rays as a greyish-white mass.
However, chest X-rays cannot provide a definitive diagnosis, as it is not possible to differentiate between cancer and other diseases, such as lung abscess (a collection of pus that forms in the lungs).
If it is lung cancer, you will have more tests to determine how far the tumour has spread.
A CT scan is usually performed after the chest X-ray.
Before such an examination, you will be given a drink or injected with a slightly radioactive contrast substance. The contrast substance makes the lungs appear clearer on examination. The scan is painless and takes 10-30 minutes.
This may be performed if the CT scan results show that you have cancer at an early stage.
The PET-CT scan can show where there are active cancer cells. It helps in diagnosis and treatment.
If your CT scan shows that there may be cancer in the central part of your chest, you will have a bronchoscopy. Bronchoscopy is a procedure that allows a doctor or nurse to harvest a few cells from the lungs.
During a bronchoscopy, a thin tube called a bronchoscope is used to examine the lungs and collect a sample of cells (biopsy). The bronchoscope is passed either through the mouth or nose, down the throat and into the airways of the lungs.
The procedure is not comfortable, but beforehand you will be given a mild sedative to help you relax and a local anaesthetic to numb your throat. The procedure is very quick and only takes a few minutes.
If for some reason you are unable to have a bronchoscopy, it is possible to have a sputum cytology examination instead. It involves taking a sample of sputum, which is then analysed microscopically for the presence of cancer.
A percutaneous punch biopsy involves taking a sample from a suspected tumour mass to be analysed in the laboratory for the presence of cancer cells.
The physician performing the image-guided biopsy will locate the tumour and guide the fine needle percutaneously to the tumour. A local anaesthetic is used to numb the surrounding skin and the needle is inserted through the skin into the lungs. The needle will then be used to take a tissue sample for microscopic analysis to determine the nature of the tumour.
Thoracoscopy is a procedure that allows the doctor to examine a specific region of the chest and collect tissue and fluid samples.
A general anaesthetic may be needed before performing the thoracoscopy. Two or three small cuts will be made in the chest to pass the tube (similar to a bronchoscope) into the chest. The doctor will use the tube to examine the inside of the chest and collect samples. The samples will then be sent for analysis.
After thoracoscopy, you may need to stay in hospital overnight while any other fluid in your lungs is drained.
Thoracoscopy is usually performed for tumours that remain undiagnosed even after bronchoscopy or image-guided biopsy.
A mediastinoscopy allows the doctor to examine the region between the lungs and the centre of the chest (mediastinum).
For this test you will need a general anaesthetic and to stay in hospital for several days. The doctor will make a small cut at the base of your neck to insert a small tube into your chest.
The tube is fitted at the end with a video camera, which allows the doctor to view the inside of the chest. Cell and lymph node samples can also be taken at the same time. Lymph nodes are tested because they are usually the first place where lung cancer spreads.
Once the above tests have been carried out, it is possible to determine the stage of the cancer, the method of treatment and whether the cancer can be completely treated.
The stages of non-small cell lung cancer are listed below.
Stage I
The cancer is in the lung and has not spread to adjacent lymph nodes:
Stage II
The tumour – at this stage – has spread to nearby lymph nodes.
Stage III
Tumora poate fi foarte mare și poate invada alte organe din apropierea plămânilor.
De asemenea, acest stadiu poate să indice și o tumoră mai mică, dar însoțită de celule canceroase în ganglionii limfatici situați mai departe de plămâni. În funcție de răspândirea tumorii, cancerul pulmonar de stadiul III se clasifică în:
Stadiul IV
În Stadiul IV, cancerul se extinde și la celălalt plămân, urmând să se răspândească și în alte părți ale corpului (oase, creier, ficat).
Small cell lung cancer has only two possible stages:
Surgery is not usually used to treat this type of lung cancer because the tumour has already spread to other areas of the body by the time of diagnosis. Only if the cancer is found very early can surgery be used.
The two types of lung cancer are treated differently, as follows:
Non-small cell lung cancer (non-small cell)
This type of cancer can be treated using surgery, chemotherapy and radiotherapy.
Small cell lung cancer
Small cell lung cancer is usually treated with chemotherapy, either alone or in combination with radiotherapy. Often this method prolongs life and relieves symptoms.
Surgery is not usually used to treat this type of lung cancer, as the tumour has already spread to other areas of the body by the time of diagnosis. Only if the cancer is found very early can surgery be used.
To reduce the risk of cancer recurrence, chemotherapy or radiotherapy may be used after surgery.
The main treatments for lung cancer are:
Other newer treatments include:
The main treatments for lung cancer are:
Other newer treatments include:
There are three types of lung cancer surgery:
Complications of lung surgery can include:
Radiotherapy is a type of treatment that uses pulses of radiation to destroy cancer cells.
A more intensive course of radiotherapy, known as radical radiotherapy, may be used to cure non-microcellular lung cancer if the person is not healthy enough for surgery.
Radiotherapy can be used after surgery or it can be used to control symptoms and slow the spread of cancer when a cure is not possible (this method is known as palliative radiotherapy).
A type of radiotherapy known as prophylactic cranial irradiation (PCI) is also used to treat small cell lung cancer. CPI involves directing high-energy pulses to the brain.
This type of radiotherapy is used as a preventative measure because there is a risk of small cell lung cancer spreading to the brain.
With the latest IMRT technology, and even more so with the latest VMAT technology, there is now the possibility to protect the organs at risk that are close to the tumour from being affected by the treatment itself, while at the same time being able to deliver high doses to the diseased areas. With the level of precision of VMAT technology, non-operable lung cancers can now also be treated.
Side effects of radiotherapy include:
Side effects should pass once the radiotherapy session is completed.
Chemotherapy uses powerful cancer cell-killing drugs to treat cancer. There are several different ways chemotherapy can be used to treat lung cancer. For example, these may be:
Chemotherapy treatments are usually given in series. One series involves taking chemotherapy medication over several days and then taking a break for a few weeks to allow the body to recover from the effects of treatment.
The number of rounds of chemotherapy you need will depend on the type and extent of your lung cancer. Most people need 4-6 courses of treatment over 3-6 months.
Chemotherapy for lung cancer involves a combination of different drugs. The drugs are usually administered by infusion into a vein, or through a tube that is connected to one of the blood vessels in the chest.
Side effects of chemotherapy may include:
These side effects should gradually wear off as treatment is completed, or you can take other medicines that may make you feel better during chemotherapy..
Chemotherapy can also weaken your immune system, making you more vulnerable to infection. Inform your care team or doctor as soon as possible if you show possible signs of an infection, such as: